Gallbladder stones


Gallstone disease is common, with prevalence of 10-15% of the population in developed countries. Surgery is necessary if they cause symptoms such as bloatedness after food and abdominal pain, or if they cause complications such as infection, bile duct obstruction, and pancreatitis (inflammation of the pancreas which may be severe and life-threatening). Your doctor may ask you to go for a gastroscopy before deciding for surgery, because the symptoms for gallstone disease and gastric conditions may overlap.
Gallbladder surgery is routinely done with minimally invasive key-hole or laparoscopic surgery. This is the gold standard and allows rapid recovery and return to work with minimal or no need for hospitalization.
When the gallbladder is acutely infected (acute cholecystitis), the common approach is to wait for several weeks before surgery. However, it has been shown that early laparoscopic cholecystectomy (ELC) during the same hospital visit will lead to shorter stay in hospital and faster return to work, as well as avoiding the risk of repeat infection while waiting for the delayed surgery. In such cases, it is crucial to have a surgeon who is very experienced with the procedure to avoid complications such as injury to surrounding structures especially the bile duct.
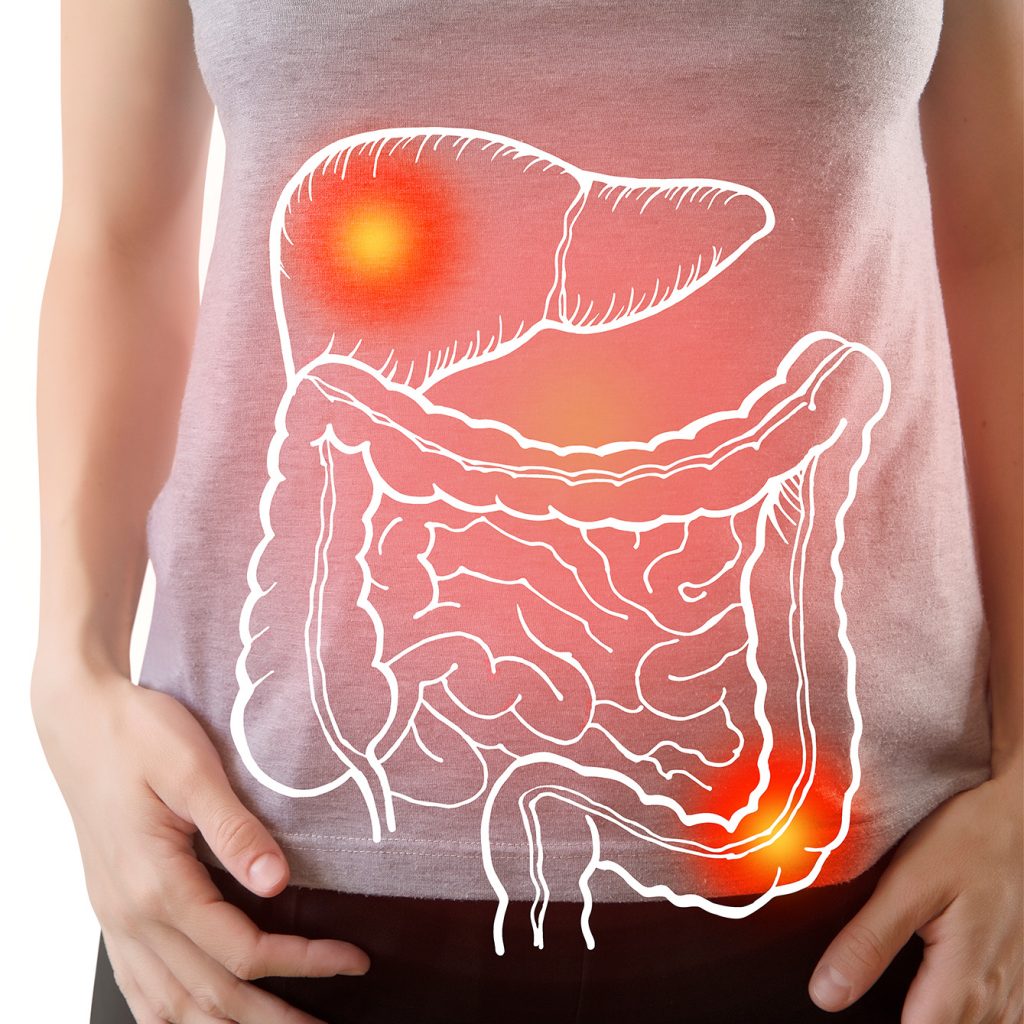
Bile duct stones
Stones in the bile duct commonly arise from the gallbladder. It may get lodged in the bile duct, leading to jaundice (yellowing of the eyes, often with tea-coloured urine and pale stools). Infection can quickly set-in (cholangitis), and typically leads to septic shock and death if not treated promptly. It is crucial to urgently decompress the blocked biliary system. This can be done by:
1. Endoscopic Retrograde Cholangio-Pancreatography (ERCP), which is an endoscopic procedure done under sedation. During ERCP, bile duct stones can be removed, or a stent inserted to allow bile drainage.
2. Percutaneous Transhepatic Biliary Drainage (PTBD). This is performed by the radiologist, where a tube is inserted through the abdominal wall into the liver and bile duct to allow drainage of the bile. The disadvantage of PTBD is mainly the discomfort associated with the external tube. However, in a very ill patient, PTBD may be more suitable.
In some patients, bile duct stones are detected during routine checks before or during gallbladder surgery. There may not be any obstruction or jaundice present, and the patient is well. If possible, ERCP should be done to remove the bile duct stones before gallbladder surgery. In suitable cases, the bile duct stones can be removed at the same time during laparoscopic cholecystectomy (laparoscopic common bile duct exploration).
Dr Tan possesses the complete skill set to treat biliary stone disease, being proficient with surgical options as well as ERCP.
Liver Cancer

Cancer of the liver is divided into primary liver cancer and secondary liver cancer.
Primary liver cancer arises from the liver itself. Examples are hepatocellular carcinoma (HCC) and cholangiocarcinoma.
Globally, HCC is the 6th most common cancer but the second most common cause of cancer-related death. In Singapore, HCC is the 3rd most common cause of cancer-deaths in males and 4th most common in females.
Patients with hepatitis B, hepatitis C and alcoholic liver cirrhosis are the main at-risk groups for developing HCC. Because early HCC is usually without symptoms, many patients present at an advanced stage where curative treatment is not possible. Hence it is important for at-risk patients to receive regular screening tests to detect HCC at an early stage when cure is still possible.
Curative treatment for HCC involves surgical resection of the tumor, or liver transplantation.
- -Certain of the diagnosis and extent of surgery needed
- -Determine the functional capacity of the liver in order to prevent severe complications after surgery.
- -Optimize patient’s condition pre-operatively to improve safety and outcomes.
This requires a multidisciplinary approach involving Radiologist, Hepatologist, Anesthetist with experience in conducting anesthesia for liver surgery, and dedicated Nursing staff and facilities. Dr Tan will coordinate care between these professionals for the best outcome for the patient.
With improved techniques and peri-operative care, liver resection has a mortality rate of less than 5%, and confers 5 year survival rates of up to 60%.
Secondary liver cancer refers to cancer arising elsewhere but metastasize (spreads) to the liver. Of these, liver resection is commonly performed for metastases from colorectal cancer (read more…) and neuroendocrine cancer (read more…).
Colorectal cancer liver metastases (CRM)
Colorectal cancer (CRC) is the leading cancer in men, and the second commonest cancer in women in Singapore. 50% of patients with CRC develop CRM. Surgical resection of CRM is the only potentially curative modality. Together with effective systemic chemotherapy, a 5-year survival rate of between 40 to 60% can be achieved.
Neuroendocrine tumor (NET) metastases
Neuroendocrine tumours (NET) are a group of tumours most commonly found in the gastrointestinal tract. They can produce a variety of symptoms due to the production of hormonal substances. About 80% of patients with NET develop liver metatstases, usually at the time of diagnosis.
Many patients can still have prolonged survival despite metastases to the liver. When untreated, 20-40% of patients can survive for 5 years or more. However, if the primary source of the tumour as well as the liver metastases can be completely removed, the percentage of patients surviving for 5 years or more increases, up to 80%. This is despite recurrence being common after liver resection.
In patients whereby not all of the tumour can be removed, some will still benefit from surgery to remove most of the tumour (cytoreductive surgery) to alleviate symptoms due to secretion of hormones by the tumour or from swelling of the liver.
Pancreatic Cysts/Tumours

Pancreatic surgery is done for cancer of the pancreas as well as other lesions such as cysts that may be pre-cancerous. Growths on the left side (body and tail) of the pancreas will be removed via a distal pancreatectomy, whereas growths on the right side (head of pancreas) necessitate a Whipple’s operation.
Distal pancreatectomy can often be done minimally invasively with laparoscopic surgery with good outcomes.
Whipple’s operation is a major operation usually reserved for the HPB surgeon. For pancreatic cancer, successful removal of the tumor offers the only chance for cure. With modern surgical and anesthetic techniques, safety has improved greatly with reduced mortality rate but complications are still common. An experienced surgeon is therefore essential to keep complications to the minimum.
